More than ever before, people are talking about mental health. We have mental health days. We listen to podcasts about finding the perfect balance in our lives to preserve our mental health. We read books about what foods to eat and activities to do to maintain or improve our mental health. But what do we really mean by “mental health?” Our mental health is essentially the overall state of our mood and psychological well-being. For each of us, our mental health greatly impacts our functioning, our productivity, and our relationships with others.
The increased focus on mental health in our society is a welcome change to the decades of shame and secrecy associated with experiencing a mental health struggle. However, it can still feel confusing or sometimes even scary to have a diagnosis attached to us or a loved one. While we’ve made a lot of progress in fighting stigma, we still have a ways to go. This is one of the reasons why it’s so important to understand what “diagnosis” means and why we focus on them in mental health treatment.
What does “diagnosis” mean within the context of mental health?
A diagnosis is a word or words assigned to a set of behaviors and feelings. The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision (DSM-5-TR) was published in 2022 and is compiled using input from over 200 mental health experts. This is the text mental health professionals use to determine what a set of symptoms means and to understand the severity of the symptoms so we can establish the best plan of action. Exploring diagnoses is important in choosing pharmacological and/or other kinds of treatment in order to help people better cope with their symptoms and engage more fully in their lives.
Some common diagnoses fall under the Anxiety umbrella, such as Generalized Anxiety Disorder, Social Anxiety, and Obsessive-Compulsive Disorder. There are also mood disorders like Major Depression and Bipolar Disorder. Trauma disorders are also categorized in the DSM. Each of these has a set of criteria that looks at what’s happening internally and physiologically over a specific period and how these symptoms impact one’s functioning and relationships. For instance, Generalized Anxiety Disorder is “marked by excessive anxiety and worry occurring more days than not for at least 6 months causing clinically significant distress or impairment in social, occupational, or other important areas of functioning (DSM-5-TR).”
Now, let’s take a deeper look at some of the diagnoses treated at Compass.
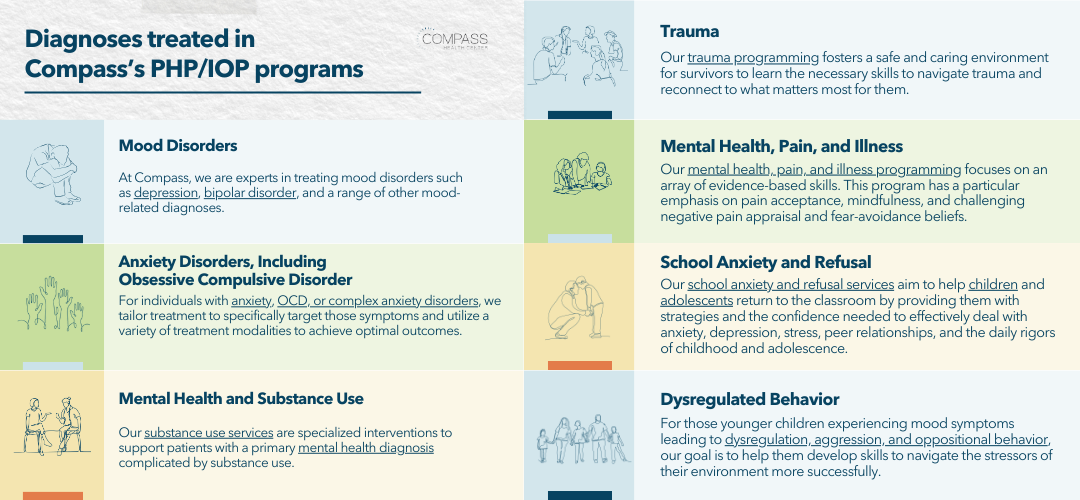
Diagnoses treated in Compass’s PHP/IOP programs
Mood Disorders
At Compass, we are experts in treating those with mood disorders such as Depression, Bipolar Disorder, and other related diagnoses. Our therapists are specialists in evidence-based therapies proven to be the gold standard for treating these conditions. Through closely monitoring our patient outcome measures, we know that we are seeing a clinically and statistically significant decline in symptoms in our patients at discharge versus when we first meet them.
Anxiety Disorders, Including Obsessive Compulsive Disorder
For individuals with anxiety, OCD, or complex anxiety disorders, we tailor treatment plans to specifically target those symptoms. Research shows that one of the most effective treatments for OCD and complex anxiety diagnoses is exposure therapy. Our trained exposure therapists help patients gradually confront their feared object or situation, so people learn to better manage their anxiety and fears. This treatment is complemented by cognitive behavioral therapy, dialectical behavior therapy, and acceptance and commitment therapy.
Mental Health and Substance Use
Our substance use services are specialized interventions to support patients with a primary mental health diagnosis complicated by substance use. We rely on both abstinence-based and harm-reduction models to treat substance use. We specifically fit our substance treatment to the individual to allow them to make the most progress on their goals.
Trauma
Our trauma programming fosters a safe and caring environment for survivors to learn the necessary skills to navigate trauma and reconnect to what matters. In addition to our other evidence-based treatments, we utilize Cognitive Processing Therapy (CPT). CPT applies Cognitive Behavioral techniques directly to the traumatic experience to work through the residual effects.
Mental Health, Pain, and Illness
Our mental health, pain, and illness programming focuses on an array of evidence-based skills. This program has a particular emphasis on pain acceptance, mindfulness, and challenging negative pain appraisal and fear-avoidance beliefs. Sessions consist of personalizing and applying skills and setting goals related to managing mental health symptoms in the context of pain and / or illness.
School Anxiety and Refusal
Our school anxiety and refusal services aim to help children and adolescents return to the classroom by providing them with strategies and the confidence needed to effectively deal with anxiety, depression, stress, peer relationships, and the daily rigors of childhood and adolescence. Specific assessments are conducted to understand the underlying factors contributing to the refusal behavior. Individualized treatment plans addressing psychiatric symptoms, behavior, and goals are developed by the multi-disciplinary team in collaboration with children and their families.
Dysregulated Behavior
For those younger children experiencing mood symptoms leading to dysregulation, aggression, and oppositional behavior, our goal is to help them develop skills to navigate the stressors of their environment more successfully. Our staff is certified through the Crisis Prevention Institute in crisis prevention and intervention to maintain the most therapeutic environment in our milieu. While in treatment, we provide various therapies that will improve the child’s functioning by gaining strategies and learning how to utilize them effectively.
You are not alone – 1 in 5 adults and 1 in 6 youth struggles with mental health
If you or a loved one is struggling with a mental health disorder, it is important to know – you are not alone. According to the National Alliance on Mental Illness (NAMI), 1 in 5 adults in the United States experience a mental health struggle each year. And these struggles don’t only affect adults; children and adolescents are also impacted by mental illness. NAMI cites 1 in 6 youth in the United States experience a mental health episode each year.
For some, suicidal thoughts can accompany other symptoms when one is experiencing a mental illness. Suicide is the 2nd leading cause of death among people aged 10-14, the 3rd among those 15-24, and the 12th leading cause of death overall in the United States (NAMI). Talking about suicidal thoughts, checking in on one another, and seeking treatment can produce a lifesaving impact. What we know is -the treatment for mental health is more effective than ever. There are countless medications, treatment modalities, interventions, levels of care, and mental health providers-- suicide does not need to be the answer. We know that relief from the overwhelming weight of mental illness is possible.
Levels of mental health treatment
Seeking treatment for a mental health condition can feel daunting, although treatment is more accessible now than ever before, especially with parity laws. Working closely with a primary care doctor or mental health professional to determine the best level of care for you or your loved one is the first step. Level of care refers to the intensity of the treatment that is sought. Intensity is impacted by the professionals involved, the time spent in treatment, and the modalities used. The least intense level of care is also probably the most familiar. This is treatment in outpatient therapy where one is meeting with an outpatient therapist with some level of frequency- every other week or weekly is most common. Sometimes this is accompanied by meetings with a psychiatrist or prescribing physician or nurse to discuss medications. The most intense level of care involves “living” in the treatment setting. This might look like a short-term stay in the hospital for stabilization or longer-term treatment in a residential facility.
Compass’s PHP/IOP level treatment model
When more intensive treatment is needed than regular outpatient therapy, but one does not need to be "living” in the treatment space, partial hospitalization (PHP) or intensive outpatient (IOP) programs are often sought. Specifically, PHP is meant to be a short-term focus on mental & emotional health needs when one is not able to fully function in their typical routine. While IOP does allow people to remain engaged in most activities in their life, they are also engaging in intensive therapy. These are the programs offered at Compass Health Center. These treatment levels allow people to remain engaged in their lives as they spend several hours in treatment in a week but remain in their usual living situation.
At Compass, a focus on learning evidence-based coping skills stemming from Cognitive Behavioral Therapy (CBT), Dialectical Behavior Therapy (DBT), and Acceptance and Commitment Therapy (ACT) in a group setting are the “anchors” of these two types of programs. Individual meetings with a primary therapist help reinforce these skills and individualize treatment even more to each person and set of symptoms. An emphasis on engaging one’s support system in Family or Couple’s Therapy is also encouraged. For our child and adolescent patients, educational specialists provide assistance in managing one’s academic needs. Finally, working closely with a psychiatrist or psychiatric nurse practitioner to explore medications as well as diet, exercise, and other interventions is a key aspect of PHP/IOP care at Compass.
Access to the right type of treatment saves lives
What we have seen after 11 years of treating thousands of people in the Chicagoland area is that this combination of treatment not only allows people to make significant gains in a relatively short period of time, but it also truly saves lives. While our fight continues to remove the stigma from mental health and raise awareness about incredibly impactful treatment options, we are encouraged by the strides made in the past ten years. Knowing that you or your loved one is not alone, that you are more than just a diagnostic label, that there is a promise of relief and recovery ideally brings comfort and hope. Even if it simply brings more of an openness- make that call, talk to that friend, reach out to that loved one. Connecting with the right treatment can be a life altering experience.
Want to learn more?
Further Reading:
- What is PHP/IOP?
- What is Virtual PHP/IOP?
- How Do I Know Which Type of Mental Health Treatment is Right for Me? | A Clinician’s Guide to Understanding Levels of Care
- Three Ways to Identify Emotions to Help Navigate Your Feelings | A Clinician's Guide for Improved Mental Health
.png?width=1200&height=500&name=Delay%20in%20care%20(2).png)






